Learning SBIRT with standardized patients helps students “practice saying the words themselves”
The use of standardized patients always makes a big impression on the medical students we train about substance use.
After completing the three-week Scaife Advanced Medical Student Fellowship on addiction and its treatment, one of our medical students described some initial stress when faced with a standardized patient.
“There was no time to be shy. On the second day, we were given a pair of standardized patients and asked to motivationally interview them…At first, this seemed to be quite the intimidating task. I remember walking into a brightly lit room to encounter a young woman with dark sunglasses and arms crossed, completely closed off from any interaction. What in the world was I going to say to this woman to get her to open up to me? Would she be offended by my prying into her personal life?”
He learned a lot, though—and quickly. Not just about the patient’s history, but about the dynamics that play out every day between medical professionals and their patients.
“As I sat down to speak with her, my apprehension faded and slowly I grew more confident. The ten minutes we spent delving into her abusive past and drug history opened the conversation up to a plethora of issues, but sadly the timer went off and she closed herself off once again, this time preparing for the next student. Though this was a short experience, it brought to light one of the most important barriers to effectively addressing addiction in our society today: a lack of trust.”
(Read his whole post about trust here.)
What’s a standardized patient?

You guessed it. The woman in the sunglasses did not actually experience the trauma she described to our medical student. As a standardized patient (SP), she learned a story–based on a real patient’s–and portrayed it consistently to each of the medical students in our summer Fellowship.
This gets to the heart of the unique value that SPs offer: not only are they realistic (real humans interacting in real-time), but they’re consistent–they’re standardized. This means that students can repeatedly practice essential skills like building rapport, gathering an organized and accurate history, and making appropriate clinical decisions.
Students can also discuss their responses to the SP with one another and be confident that they encountered the same symptoms, personal history, and personality traits.
How does IRETA use standardized patients?
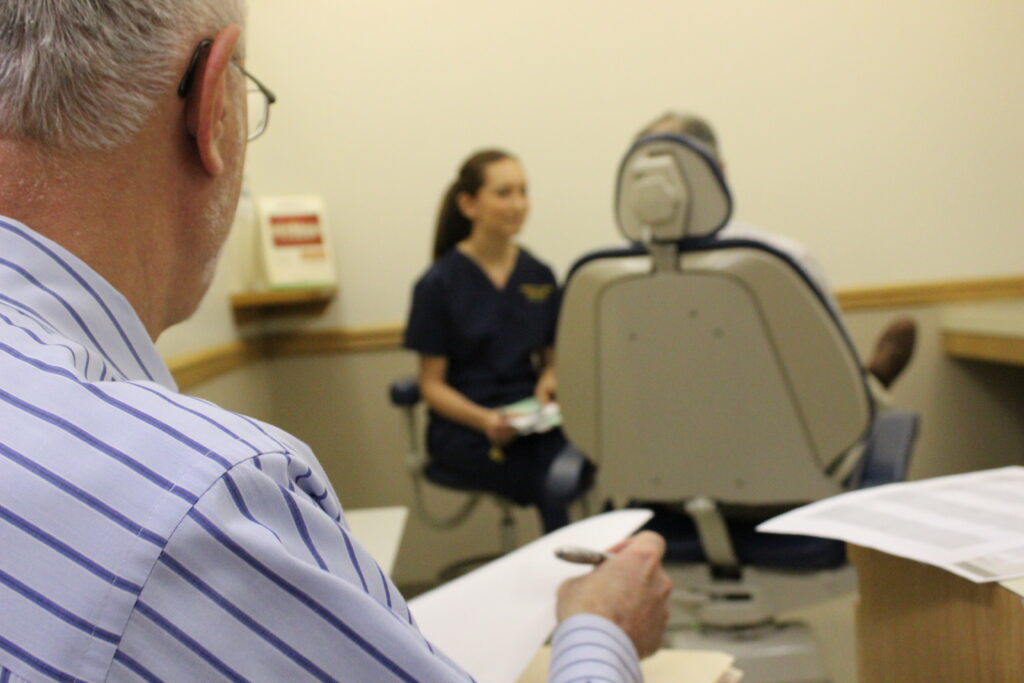
SPs are an invaluable part of our work. As a nonprofit that helps people respond effectively to substance use and related problems, one of our specialties is training health providers. We have used SPs to train medical students and dental hygiene students with such success that we’re extending our use of SPs into training for nursing students, nurse anesthetist students, dental students, and dental anesthesiology students at the University of Pittsburgh.
We use SPs to teach an intervention called Screening, Brief Intervention and Referral to Treatment (SBIRT), which is a promising public health approach to preventing and reducing risky substance use. SBIRT is a structured conversation that starts with a few screening questions to determine a patient’s level of risk. Low-risk individuals receive positive reinforcement; mid- to high-risk individuals are engaged in a conversation about substance use called a brief intervention; and some high-risk individuals are referred to specialty treatment.
“Learning SBIRT is so much about learning communication skills,” said Dr. Holly Hagle, who directs IRETA’s SBIRT training program. “We know that conversations about substance use can be uncomfortable, so it’s extremely important for students to practice responding sensitively to patients and providing them with accurate information.”
IRETA’s Research Associate Piper Lincoln agreed. “The students have to practice saying the words themselves; they can’t just sit there and watch.”
Lincoln speculated that SBIRT training is particularly well-suited to the use of SPs.
“I would argue that standardized patients are particularly important for behavioral intervention trainings because in those cases, the interaction is the healthcare—and patient interaction is complex. Everything happens very fast. So you’ve got to practice,” said Lincoln.
And Hagle has noticed that SPs help soften students’ skepticism that SBIRT takes too long.
“When the students are working with standardized patients, I intentionally time them so that we can test out what it’s possible to accomplish in ten minutes. It turns out that you can actually accomplish a lot; you can engage patients and be sensitive and empathetic with them in a ten minute managed care window.”
Starting in 2015, IRETA will use SPs to train all students who participate in the InterProfessional Groups of Anesthesia Students (InGAS) project, which emphasize the importance of SBIRT among various medical professionals who use anesthesia.
Standardized patients as cutting edge technology
In June 2015, IRETA and partners at the University of Pittsburgh will host a conference specifically designed to expand the use of SPs in SBIRT training. With workshops titled “How to Design an Educational Session with Standardized Patients” and “Implementing a Simulation Session: Key Considerations,” presenters will introduce key elements of SPs as an SBIRT training methodology for those who are interested, but not sure how to start.
The keynote speaker will Dr. Eduardo Salas, head of the Institute for Simulation and Training at the University of Central Florida. The Institute for Simulation and Training works in a number of high-tech areas—virtual reality, autonomous robots, military flight simulators, for example. But at the SBIRT conference, Salas will be talking about SPs as powerful simulation technology to improve healthcare and prevent substance use related harms.
Resources
Standardized Patient Program at the University of Pittsburgh
Registration for our June conference (lots of information and wisdom about how to use SPs in SBIRT training)
IRETA’s resources on Screening, Brief Intervention and Referral to Treatment
Scaife Advanced Medical Student Fellowship (now accepting applications for summer 2015)






